If you track and test your lipids regularly (and you should) you may have noticed either a slow creeping up or a completely out of the blue increase of your total cholesterol or perhaps just of your LDL (low density lipoprotein) cholesterol, aka the “bad” cholesterol.
If so, you are not alone. Rising cholesterol in midlife women is common. On average the increase in total and LDL can range from 10-25%. The reason: you guessed it, its our plummeting estrogen. Again.
So what exactly does estrogen have to do with cholesterol? And what the heck does cholesterol do in our bodies anyway?
This post will provide an overview of what cholesterol is, the different types and the usefulness of measuring these. We will then look at the relationship between estrogen and lipid metabolism. Finally we will look at some strategies to manage rising cholesterol.
What is cholesterol?
There are few villains in the diet and health space with a worse reputation than cholesterol. How has cholesterol become so demonised and does it deserve the bad press it receives?
First let’s get this important point out of the way – cholesterol is essential to life. So if your goal is to rid your body of cholesterol, that may not end so well!
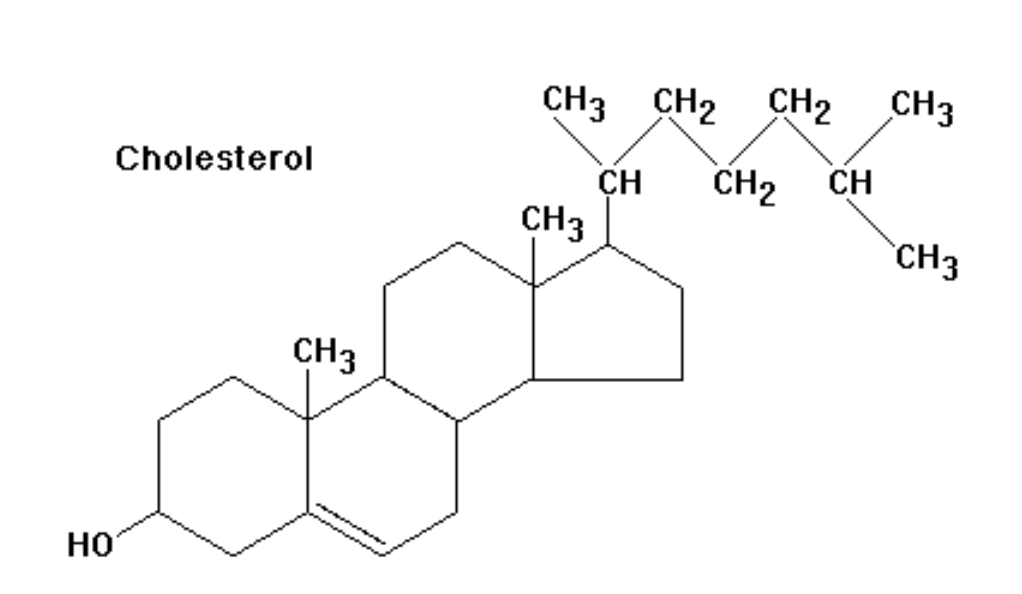
Cholesterol is vital to human survival as it is the primary component of the cell membrane of every cell in your body. Secondly it is the base or foundational building block of all the steroid hormones in our body – hello cortisol, progesterone, DHEA, testosterone, and estrogen!
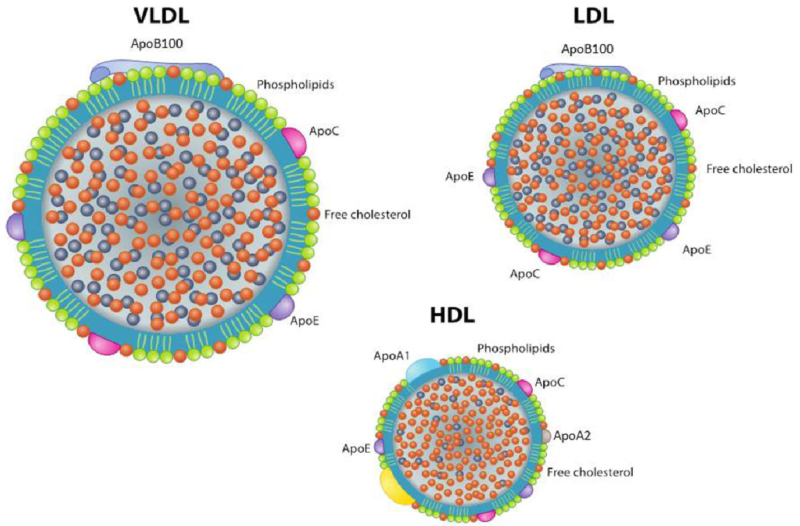
We broadly speak of cholesterol in two categories: Low Density Lipoprotein Cholesterol (LDL) and High Density Lipoprotein Cholesterol (HDL) and they have different jobs.
For simplicity sake we need to understand a couple of points:
-
LDL cholesterol particles are larger and less dense; they start in the liver and deliver the necessary cholesterol out to the rest of the body.
-
HDL, is much smaller and heavier; it transports excess cholesterol from the body, back to the liver for removal.
Given the very important role of cholesterol to the structure and functioning of our bodies, both of these forms of lipoproteins are GOOD.
So why the bad rap?
Well, when certain particles of a certain size and density bang into the sides of our blood vessels and arteries, they damage the cells lining the walls of the vessels (this lining is known as the endothelium), become embedded, inflamed, then calcified, and ultimately cause the narrowing of the passage in which blood can flow, leading to cardiovascular disease, heart attacks, and strokes.
If you guessed this evil, damage-causing culprit to be LDL, you would be (mostly) correct. Why only mostly correct ?
Well, what we measure when we measure LDL-c is how much cholesterol (shown by the orange dots above) is carried within the lipoprotein (a carrier molecule made of protein on the outside so that lipids, which are not water soluble, can move around in plasma or blood).
Does it actually matter how much of that cholesterol is contained within the lipoprotein? Not so much.
What does matter? The number of particles and the size of the particles. Think of a roadway – the likelihood of vehicles being in an accident – hitting each other or running into the guard rails (ie the endothelium), in a confined space has more to do with the size and number of vehicles, NOT how many passengers are in the vehicles. Ultimately if you want more meaningful information you should really be testing your Apo-A (corresponds to HDL) and Apo-B (corresponds to LDL) in addition to the standard lipid measurements of cholesterol, as they are more indicative of the particle number.
The next important point to make is that the vast majority (+80% of your body’s cholesterol) is endogenous – that means it is made by your body. A VERY small percentage of your cholesterol comes from the food you eat! Most dietary cholesterol is in the wrong form, and is unusable by the body unless it undergoes a chemical reaction. Who knew right? So much for the anti -egg crusade!
What does menopause have to do with increasing cholesterol levels and Cardiovascular disease?
The million dollar question is why do women in the menopause transition suddenly have sky-rocketing cholesterol levels?
The liver plays a key role in the metabolism of lipids in our bodies. It is really the hub of fatty acid synthesis (where it is made) and circulation through the body.
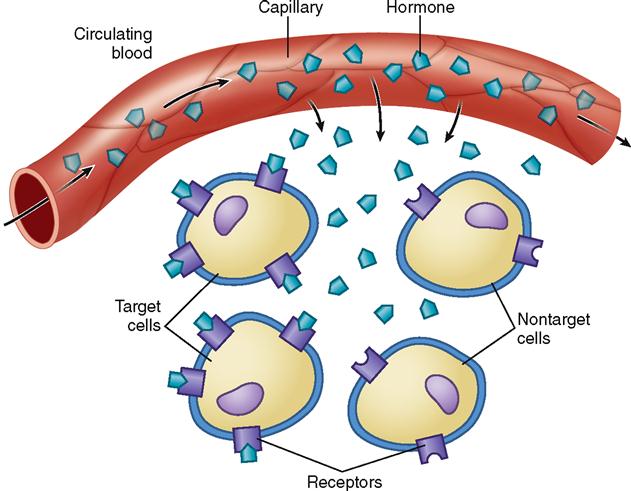
Estrogen receptors in the liver help regulate the metabolism of lipids in a complex series of reactions. For example, in simple terms this means to properly metabolise, estrogen has to attach to the cell’s receptor. The drop in estrogen levels during menopause leads to higher circulating LDL cholesterol and triglyceride levels because where once abundant estrogen (estradiol in particular) would “dock” onto a receptor on a cell involved in lipid metabolism in the liver in order for lipid metabolism to work properly, that cell’s ability to “activate” lipid metabolism is now hindered without the estrogen, thereby leading to an increased amount or a build up lipids.
In addition, once there is some damage to our vessels caused by too many LDL ‘cars’ on the road, estradiol also plays an important role in supporting the immune system and the inflammatory response. Once estradiol decreases, we lose an important component of the immune response making the damage worse than it may have been with sufficient estradiol levels.

What can we do?
We can’t stop menopause but we can control somethings externally.
-
HRT – to increase estradiol levels -Estradiol helps to increase expression of LDL receptors which helps increase clearance of LDL. Estradiol, in most cases, can not be taken on its own – make sure you discuss with your physician whether HRT could work for you, and what forms you require.
-
Increase soluble fiber – soluble fiber binds to excess cholesterol in the intestines which can then be excreted. Additionally, the digestive process requires bile acids, which are made partly with cholesterol. As your digestion improves from eating sufficient dietary fiber, the liver pulls cholesterol from the blood to create more bile acid, thereby reducing the amount of LDL cholesterol.
-
Decrease saturated fats – not because they contain cholesterol, but because excess saturated fats cause the liver to reduce expression of LDL receptors thereby reducing the amount of LDL than can be removed from circulation.
-
Eat phytoestrogens which contain structures that are very similar to the structure of the estradiol we produce in our bodies, derived from plants. These mimic estrogen and bind to estrogen receptor sites in the liver helping to metabolise lipids. Food sources include soybeans, garlic, celery, carrots, potatoes, rice, wheat, red clover, sweet potatoes, fruits (apples, pomegranates and chaste berries) and coffee. Isoflavones are found in legumes, especially soybeans. Flaxseeds are the main source of lignans. (Pub med study.).
-
Try supplements: Red Yeast Rice, Berberine, CoQ10, and probiotics which have been clinically proven to reduce LDL by: inhibiting the amount of cholesterol synthesized in the liver, indirectly causing an increase in availability of LDL-receptors in the liver, and possibly by increasing the liver’s excretion of bile acids, thereby increasing the need for cholesterol to be used for the synthesis of additional bile.(Pub med study)
-
Mediterranean Diet – anti- inflammatory diet -increase monounsaturated fats, omega 3 fatty acids
-
Exercise daily – studies show that engaging muscles improves lipid metabolism. ( Pub med Study)
-
Medication such as Statins prescribed by your physician.